Abstract
Introduction: Acute Myeloid Leukemia (AML) outcomes have improved over time, however end-of-life care for patients with AML is suboptimal with a low utilization of palliative care and hospice services. We analyzed AML mortality cause from 2000 to 2019 using the Mortality Data from the Centers of Disease Control and Prevention (CDC). Among AML deaths, we evaluated differences in place of death, cause of death and sociodemographic characteristics including gender, race and resident status.
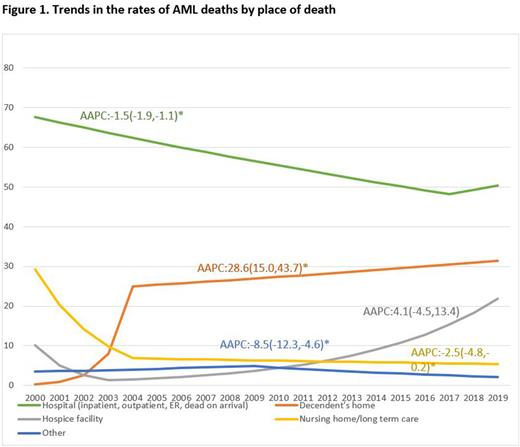
Methods: We conducted a retrospective cohort study using the Multiple Cause of Death Mortality Data from the National Vital Statistics System of the National Center for Health Statistics from January 1st 2000 to December 31st 2019. We obtained demographic characteristics of all the deaths during this period and those with AML. Among AML deaths, we examined principal cause of death and then used joinpoint regression to calculate trends in the rates of AML deaths by their location, which was represented using average annual percentage change (AAPC).
Results: 195,923 AML deaths were captured from 2000 to 2019, from more than 50 million total deaths during this timeframe. At least 85.3% of AML deaths were attributed to AML (index cancer) and 2.7% of deaths were attributed to infection. 56.0% of AML deaths occurred in hospitals, 24.7% in decedent's homes, 7.5% in hospice facilities and 8.3% in nursing homes or long term care facilities. 56.6% of AML deaths were in males. 83.1% of AML deaths were in Non-Hispanic Whites (NH-White), 7.7% in NH-Blacks and 5.8% in Hispanics. 68.8% of AML deaths were residents of state in which the death occurred and 30.9% were in non-residents. Over the studied period, there was a statistically significant decrease in AML deaths in the hospital setting with AAPC (95% CI) being -1.5 (-1.9,-1.1) and nursing home setting AAPC (95% CI): -2.5 (-4.8, -0.2) along with a statistically significant increase in AML deaths at home with AAPC (95% CI): 28.6 (15.0, 43.7) (Figure 1). The AAPC for deaths in hospice facilities was statistically non-significant.
Conclusions: Most AML deaths continue to occur in the hospital setting despite a statistically significant increase in deaths at home and trend of increased utilization of hospice facilities. Patients undergoing induction therapy for new or relapsed disease may be at higher risk of death from complications from their disease or therapy and die in the hospital setting. Young age at diagnosis, delayed goals of care discussions and hesitancy to forego transfusions may contribute to increased AML deaths in the hospital setting. This is the largest population study to date evaluating AML deaths to our knowledge, however we are limited by lacking information on the risk stratification of the AML, treatment received and circumstances of home death. We are also unable to determine the timing of goals of care conversations, whether or not patients were offered palliative care services or the timing of the hospice referral when it did occur.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.